BMJ 2023 381 p475 [Help Offered To Mary Shaniqua]
Mary Shaniqua gives neither age nor phenotype. I applaud the description of her sickle cell crisis pain, and her definition of empathy as doctors listening to her and engaging her “in decisions about my treatment.” She is “much more than a sickle cell patient” [1] because sickle cell disease patients possess non-sickling genes that equip them for achievement. But what precipitates Shaniqua’s crises? [2]
SICKLE CELL DISEASE PATIENT ACHIEVERS (SCDPA) ELIMINATED CRISES BY PREVENTING CAUSES
I organized 3 international conferences – first at Royal Society of Medicine 1993, second in Accra 1995, and the third at Accra in 2010 for SCDPA [3-6] to commemorate 100th anniversary of James Herrick’s observation [7] of sickled erythrocytes in a Black anaemic patient suffering from the hereditary condition that Ghanaians had known for centuries [8-11] by onomatopoeic tribal names [12] reflective of Mary Shaniqua’s description – “stabbing, like knife in the bones”.
IRON OVERLOAD, HIP NECROSIS, AND EMBOLISM COMPLICATIONS
Mary Shaniqua’s three “very challenging symptoms and diagnoses” [1] occur in all 4 disease-phenotypes SS SC Sbeta-Thalassaemia SF-hereditary [9-11 13 14].
(a) Iron-Overload develops in regularly transfused Sickle Cell Anaemia (SS) patients [9-11]. Supervising the world’s largest Sickle Cell Clinic at Korle Bu Teaching Hospital in Ghana I never regularly transfused any “SS” patient [9-11 13-16]. Nor did Graham Serjeant running the world’s second largest Sickle Cell Clinic in Jamaica [17-23]. Indeed, Graham Serjeant’s never-been-transfused “SS” patient on holiday in the USA died there when doctors transfused her [23]. Shaniqua’s listening doctor empathy-definition was reflected when more than once I obeyed this request: “My crisis comes when Hb is above 9 grams so please test and remove blood” [10 – Case History 21). Two world-class Consultant Haematologists I know may well write to BMJ to say they obeyed another patient of mine who pleaded for venesection when Hb approached 9 grams.
(b) Articular bone necrosis [24-26] occurred in 6.6% of my 563 sickle cell haemoglobin C disease (SC) patients and 2.8% of 583 sickle cell anaemia (SS) consecutive patients
reflecting SC phenotype’s higher blood viscosity with more mobility to greater disposition. [10 p 239] Shaniqua’s red-cell overload with articular bone necrosis suggests “SS” phenotype.
(c) Pulmonary Embolism [27] can occur in all disease phenotypes when haematocrit rises. Misdiagnosed as sickle cell crisis in an SC woman, diamorphine was given intravenously, and the patient died promptly [28].
KNOWING CAUSES OF CRISIS DIMINISHES HOSPITALISATIONS DRASTICALLY
No precipitating cause, no sickle cell crisis. [2 10 11 13]. I mentioned Blood Transfusion 58 years ago among 17 causes of sickle cell crisis [29] My SS-phenotype patient Case 21 among 133 Case Histories [10/11] had the exact complications Shaniqua had. Precipitating causes for his 5 crisis-admissions were pneumonia, typhoid fever, infected gallstones, pushing a car uphill, and thunderstorm. Crisis pain disappeared when he was hydrated and “treated with antibiotics, paracetamol, intravenous magnesium sulphate, and oral sodium bicarbonate” [10/11]. Graham Serjeant [21-23 30] and I [31-43] reject NICE’s recommendations on opiates, hydroxyurea, and regular transfusion. Prime Minister Gordon Brown’s NCEPOD Experts wrote: “In 2 years 9 out of 19 sickle cell crisis admissions died from overdose of opiates” [40-48].
RESPONDING TO FOLLOWING QUESTIONS WILL HELP SHANIQUA [49-85]
Cause of crises? Haemoglobin Phenotype? Transfusions? Opiates? Gall-stones? G6PD-Status? Pregnancies? Hydroxyurea? Numb-lower-lip (Kanumblll) Sign? Vitreous Bleed? Nosebleeds? Leg ulcers? Gnathopathy? Weather-Influence? Tummy-ache? Yellow-eyes? cocacola-coloured-urine? Osteomyelitis? Crizanlizumab? LentiGlobin? COVID-19 Vaccines?
Some SCDPA took “Aerobic Oxygen” drops between meals to prevent crises for decades [6] Would BMJ publish their stories too? What prevents UK licensing Aerobic Oxygen? [44-46]
Competing Interest: I am second of my Trait Parents’ 11 children, 3 of whom had sickle cell disease. I knew more about the sickle cell disease patient in my Manya Krobo Tribe in Ghana before I went to Medical School than most of my teachers in England did. Names of my family members suffering from sickle cell disease (HEMKOM = BODYBITING, similar description to Mary Shaniqua’s) are shown for every generation right back to 1670 AD [8-11]. Coming from a family with 3 Sickle Cell Disease siblings I find it very difficult to remain detached when the received wisdom in the management of these patients that was proven by NCEPOD to be harmful is still endorsed by NICE. Shaniqua says she needs help. The many detailed references are meant to help her join the SCDPA who have avoided many hospitalisations and have achieved a great deal in life. Clinical Experience, not Haematological experience or Genomic experience was what produced SCDPA by distinguishing the vital difference between “Treating Sickle Cell Disease” and “Managing Sickle Cell Disease Patient” [9-11 35]. When Dr Helen Ranney MD PhD, Professor of Medicine and Haematology at Albert Einstein University Medical College, New York, New York said (and published) “There is no single clinical experience in the United States comparable to that of Dr Konotey-Ahulu” [13 page 320] she was confirming my frequent claim that the DNA that made my patients become ACHIEVERS was good Doctoring, good Nursing, Good Anti microbials [10/11]. Clinical Experience made me criticise in England the received wisdom that “Sickle Cells Protect Against Malaria”. No, I said, when (in 1940) my younger brother would be running about naked aged 7 years, screaming with bodily pains and with priapism exposed to the world, our mother would calmly announce: “Tei has got malaria. Bring the bottle of Quinine quickly!”. Malaria always precipitated my brother’s sickle crisis with priapism. Malaria treated, and crisis disappeared. Prevent malaria and prevent major cause of sickle cell crisis in Africa. Prevent her noted causes of crisis and Shaniqua will visit hospital less often.
Twitter@profkonoteyahul felix@konotey-ahulu.com or www.sicklecell.md
Felix I D Konotey-Ahulu FGA MB BS MD(Lond) DSc(Hon UCC) DSc(Hon UH) FRCP(Lond) FRCP(Glasg) DTMH(L’pool) FGCP FWACP FTWAS ORDER OF THE VOLTA (Officer) Kwegyir Aggrey Distinguished Professor of Human Genetics University of Cape Coast, Ghana; Former Director Ghana Institute of Clinical Genetics, Haemoglobinopathies Consultant Physician Korle Bu Teaching Hospital, Accra and Consultant Physician Genetic Counsellor in Sickle Cell & other, Cromwell Hospital London SW5 0TU and 9 Harley Street Ltd, Phoenix Hospital Group, London W1G 9AL [www.konotey-ahulu.com or..www.sicklecell.md
References [COMPREHENSIVE To Help Mary Shaniqua become an ACHIEVER too.]
1. Shaniqua Mary. Help me manage my sickle cell pain. BMJ 2023;381:P475 April 22.
2. Konotey-Ahulu FID. The Sickle-cell Diseases: Clinical manifestations including the Sickle Crisis. Arch Internal Medicine 1974; 133(4): 611-619. [PMID: 4818434 [PubMed – indexed for MEDLINE. http://archinte.ama.assn.org/cgi/reprint/133/4/611-pdf http://archinte.ama.assn.org/cgi/content/abstract/133/4/611
3. Konotey-Ahulu FID. The Sickle Achievers (1). Ghanaian Times, July 23, 2005 “I cannot think of a single Ghanaian family that did not have or know of someone with sickle cell disease – known by Tribal names”.
4. Konotey-Ahulu FID. The Sickle Achievers (2) Ghanaian Times. August 13, 2005 “Some time ago I coined the term for cold season Rheumatism which Europeans call Sickle Cell Disease … The ACHEACHE Syndrome – ACHE from each parent”. Makes it easy for Genetic Counselling.
5. Omaboe Letitia, Konotey-Ahulu FID. The Second International Conference on The Achievements of Sickle Cell Disease Patients. Accra 19th July 1995 Conference Brochure.
6. Amanor-Boadu Dorothy, Bruce-Tagoe Alexander, Konotey-Ahulu Felix. The Third International Conference On The Achievements Of Sickle Cell Disease Patients Accra – 19th July 2010. Adeko Ltd, Accra ISBN: 978-9988-1-3927-8 “One known ‘SS’ man with a PhD, who had never in his 63 years been transfused though Hb level was never above 8.8 g/dL and who had never been prescribed Hydroxyurea, astonished delegates when he announced ‘I do not remember when I last took a pain killer for my sickle cell anaemia. Drink plenty of water, avoid malaria, and have a positive attitude to life’” [page 15] [Dorothy Amanor-Boadu was 59-year-old “SS” Nurse Oncologist]. Some ACHIEVERS took Aerobic Oxygen drops to stop crises.
7. Herrick James B. Peculiar, elongated and sickle shaped red blood corpuscles in a case of severe anemia. Archives of Internal Medicine 1910. Vol 6; pp 517-521
8. Konotey-Ahulu FID. Sickle Cell Disease In Nine Successive Ghanaian Generations For Three Centuries (Manya Krobo Tribe) In The Human Genome
Diversity Project: Cogitations of An African Native. Politics and The Life Sciences (PLS) 1999; Vol 18: No 2, pp 317-322.
9. Konotey-Ahulu FID. Pattern of Sickle Cell Disease in Ghana (A Study Of 1,550 Consecutive Patients) – A Thesis Presented For The Degree of Doctor of Medicine (M.D.) In The University Of London 1971 Awarded Feb 1972.
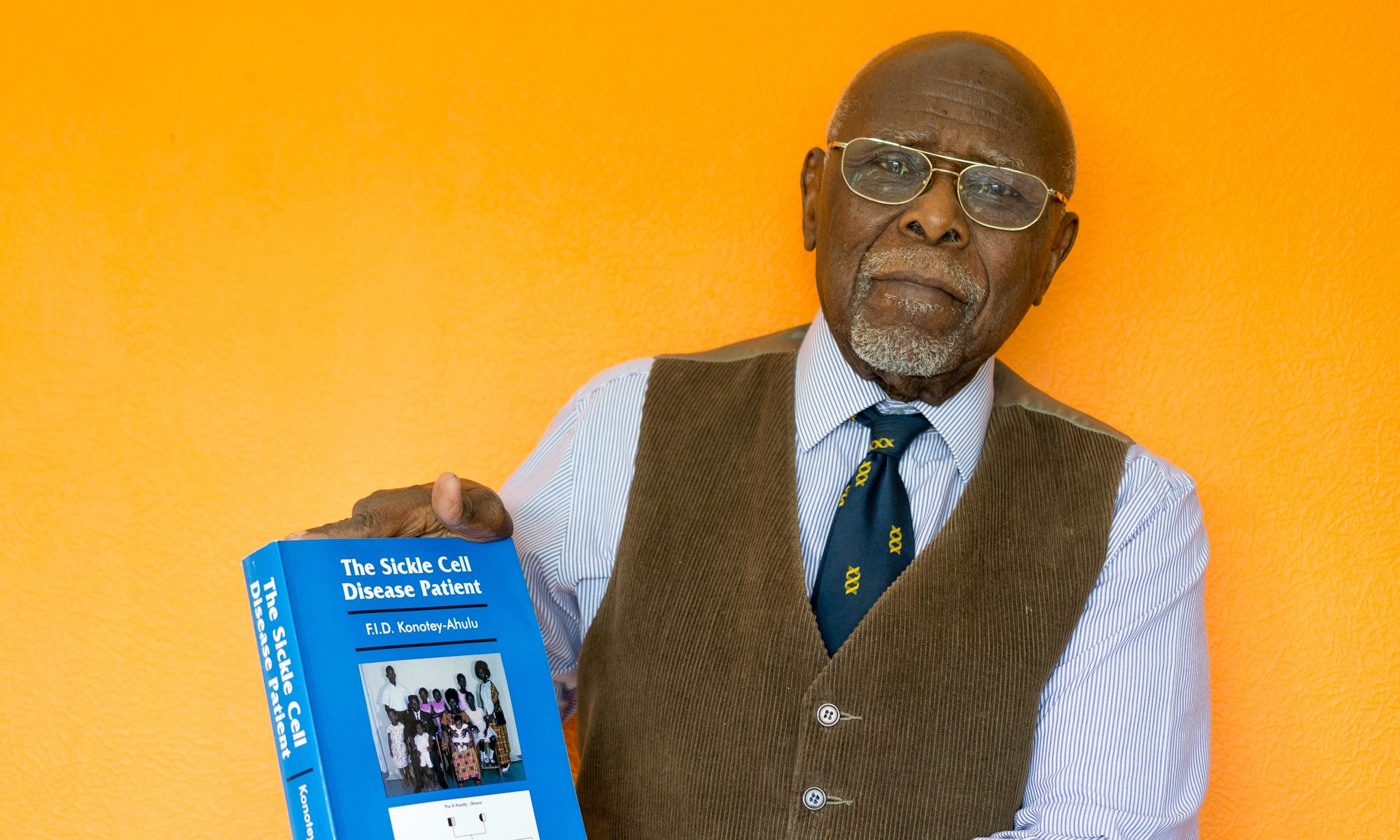
10. Konotey-Ahulu FID. The Sickle Cell Disease Patient. Natural History from a clinico-epidemiological study of the first 1550 patients of Korle Bu Hospital Sickle Cell Clinic. London & Basingstoke, Macmillan Press Ltd 1991/1992. Foreword by Roland B Scott MD, Howard University, Washington DC)
11. Konotey-Ahulu FID. The Sickle Cell Disease Patient. Clinico-epidemiological study of 1550 consecutive patients at Korle Bu Hospital, Accra. T-A’D Co, Watford 1996 http://www.sicklecell.mde/aboutscd.asp
12. Konotey-Ahulu FID. Hereditary qualitative and quantitative erythrocyte defects in Ghana – an historical and geographical survey. Ghana Med Journal. Vol 7; 118-9.
13. Konotey-Ahulu FID. Effect of environment on sickle cell disease in West Africa; epidemiologic and clinical considerations. Chapter 3 in SICKLE CELL DISEASE – diagnosis, management, education and research. Eds Ahramson, Bertles JF, Wethers Doris L; St Louis – CV Mosby Co 1973, pp 20-38 [Helen Ranney page 320: “There is no single clinical experience in the United States comparable to that of Dr Konotey-Ahulu”
14. Konotey-Ahulu FID. Patterns of clinical haemoglobinopathy. East Afr Med J 1969; 46: 149-156. (With tables that distinguish phenotypes clinically)
15. Konotey-Ahulu FID, Ringelhann B. Sickle cell anaemia, sickle cell thalassaemia, sickle cell haemoglobin C disease, and asymptomatic haemoglobin C thalassaemia in one Ghanaian family. BMJ 1969; 1: 612-614. [4 Haemoglobinopathy phenotypes] http://www.bmj.com/cgi/reprint/2/5648/48.pdf
16. Konotey-Ahulu FID. Definition of sickle cell trait and sickle cell disease. Ghana Med J 1972; 11: 417-419.
17. Serjeant GR, Richards R., Barbor PRH, Milner PF. Relatively benign sickle cell anaemia in 60 patients aged over 30 in the West Indies. BMJ 1968; 3: 86
18. Serjeant GR, Serjeant BE, Milner PF. The irreversibly sickle cell: a determinant for haemolysis in sickle cell anaemia. Br J Haematol 1969; 17: 527-533.
19. Serjeant GR. The clinical picture of sickle cell anaemia in Jamaica. MD Thesis, University of Cambridge, 1971.
20. Serjeant GR. Sickle Cell Disease. Oxford, Oxford University Press, 1985.
21. Serjeant GR. Sickle cell disease. Lancet 1997; 35: 725-730
22. Serjeant GR, Serjeant B. Sickle Cell Disease, 3rd Ed, Oxford, OUP, 2001.
23 Serjeant GR. Blood transfusion in sickle cell disease. A cautionary tale. Lancet 2003; 361: 1659-60
24. Konotey-Ahulu FID. Avascular Hip Necrosis: Sickle Haemoglobinopathy predominates worldwide. BMJ Rapid Response to Lamb JN et al 1 June 2019 Avascular necrosis of the hip. https://www.bmj.com/content/365/bmj.l2178/ BMJ 1 June Vol 365, p 325 (BMJ 2019; 365: l2178)
25. Konotey-Ahulu FID. Hip pain and radiographic signs of osteoarthritis: Sickle cell & other haemoglobinopathy differential diagnosis. British Medical Journal Rapid Response 8 January 2016 http://www.bmj.com/content/351/bmj.h5983/rr-2 to MJ Nieuwenjse and Rob G Nelissen BMJ 2015; 351 (Published 2 December 2015) http://dx.doI.org/10.1136/bmj.h5983 http://www.bmj.com/content/351/bmj.h5983/rr-2
26. Konotey-Ahulu FID. Hip disease in Africans. Lancet 1970; 1(7654): 999. http://www.biomedsearch.com/NIH/Hip-disease-in-Africans/4191955.html
27. Konotey-Ahulu FID. Pulmonary embolism, Lancet 17 July 2004 Vol 364 No 9430, pp 244-245.
28. Shoetan Cecilia. I lost my Sickle Cell Disease adult daughter minutes after being given Diamorphine intravenously when she could not breathe.
http://www.bmj.com/cgi/eletters/336/7654/1152-a#196520 BMJ June 3, 2008
29. Konotey-Ahulu FID. Sicklaemic human hygrometers. Lancet 1965; 1:1003 1004 [Listing precipitating causes of crises eg cold weather, sweating, transfusion etc] [http://www.pubmedcentral.nih.gov/picender.fcgi?artid=1846286&blobtype=pdf
30. Serjeant G. The case for dedicated sickle cell centres. BMJ 2007; 334: 477 “In Jamaican experience morphia or its derivatives are rarely used or necessary” and “the most painful crises may be treated in a day centre, the patient returning home in the evening”.
31. Konotey-Ahulu FID. Opiates for sickle-cell crisis? Lancet 1998; 351: 1438. [“The question that puzzles me is: why do west African and West Indian patients with sickle-cell disease who did without morphine in their countries have to be given morphine pumps during sickle-cell crises when they come to the UK?”]
32. Konotey-Ahulu FID. Opiates for sickle-cell crisis. Lancet 1998; 352: 651-652. [In response to David Bevan’s criticism (in Lancet 1998; 351: page 1965) of white physicians who agree with Dr Konotey-Ahulu that opiates have created addicts in their hospital – “When I say routine opiates for sickle crisis are not the way to bring out these patients’ best potential in the long term I am glad to hear white physicians say the same…White physicians who, at the risk of being misunderstood by Bevan, voice their displeasure at what they see happening on their wards deserve commendation, not condemnation.”]
33. Konotey-Ahulu FID. Opiates for pain in dying patients and in those with sickle cell disease www.bmj.com/cgi/eletters/335/7622/685#177986 BMJ Resp 11 Oct 2007
34. Konotey-Ahulu FID. Dedicated sickle cell centres. BMJ Rapid responses March 20 2007 http://www.bmj.com/cgi/eletters/335/7618/462#167455
35. Konotey-Ahulu FID. Management of patients with sickle cell disease. African Journal of Health Sciences 1998; 5: 47 [On Sally Davies and Lola Oni in BMJ 315: 656-60 “The Central Middlesex management protocol uses morphine infusions”] Response: “I fear Davies and Oni’s statement will make morphine the accepted drug for sickle crisis management. The consequences for such an approach are dire, especially when some UK hospitals are already making diamorphine their first choice”. And what did NCEPOD find in 2008?
36 Konotey-Ahulu FID Morphine for painful crises in sickle cell disease. BMJ 1991; 302: 1604 (Commenting on Professor Chamberlain’s recommendation of morphine in pregnancy in sickle cell disease – BMJ 1991; 302: 1327-30). “In obstetrics what happens too foetal respiration when morphine is used? http://www.bmj.com/cgi/reprint/302/6792/1604-c.pdf
37. Ringelhann Bela, Konotey-Ahulu FID. Haemoglobinopathies and Thalassaemias in Mediterranean areas and in West Africa: Historical and other perspectives 1910 to 1997. Accademia del Scienze Ferrara Atti, volume 74, Anno Accademico 174 1996-97, pages 297-307 [A Century Review] (Sickle Cell Disease is NOT just in Blacks)
38. Konotey-Ahulu FID. Management of acute painful sickle cell episode in hospital; summary of NICE Guidance is frightening. BMJ 2012; 344: doi:http://dx.doiorg/10 1136/bmj’e’4063 https://www.bmj.com/content/344/bmj.e4063/rr/599158 Sept 7.
39. Konotey-Ahulu FID. Management of sickle cell disease patient in the community. Rapid response 13 April 2014 [90 references] to Brousse V, Makall J, Rees DC: Management of sickle cell disease in the community, BMJ 2014; 348: g1765 doi: 10.1136/bmj,g1765 https://www.bmj.com/content/348/bmj.g1745/rr/694233 ,
40. NCEPOD – National Confidential Enquiry into Patient Outcome and Death. SICKLE: A Sickle Crisis? 2008 [Sebastian Lucas (Clinical Coordinator), David Mason (Clinical Coordinator), M Mason (Chief Executive), D Weyman (Researcher)/ Tom Treasurer (Chairman) info@incepod.org31.
41. Mason S. Enquiry shows poor care for patients with sickle cell disease. BMJ 2008; 336: 1152 “In 2 years 9 out of the 19 patients with sickle cell disease who had 9ain on admission and who then died had been given excessive doses of opiods”
42. Konotey-Ahulu FID. Poor care for sickle cell disease patients: This wake-up call is overdue. http://www.bmj.com/cgi/eletters/336/7654/1152-a#196244 BMJ Rapid Response (May 28) BMJ 2008; 336: 1152 to Susan Mayor’s “Enquiry shows poor care for patients with sickle cell disease” on National Confidential Enquiry into Patient Outcome and Death (NCEPOD) REPORT “SICKLE: A Sickle Crisis? (2008)” http://www.info@ncepod.com .
43. Konotey-Ahulu FID. Inquest into diamorphine deaths: Does NCEPOD sickle cell patients report warrant a similar inquest? BMJ Rapid Response March 7 2009 http://www.bmj.com/cgi/eletters/338/mar03_3/b903#210208
44. Goodman Elisabeth. Use of ketorolac in sickle cell disease and vaso-occlusive crisis. Lancet 1991; 338: 641-642. [Ketorolac not licenced in UK (See Ref 45)]
45. Liesner RJ, Vandenberghe EA, Davies Sally C. Analgeisics in sickle cell disease disease. Lancet 1993; 3411: 188. [Ketorolac not licensed but Diamorphine is in UK].
46.. Konotey-Ahulu FID. PAIN CONTROL: Don’t Pregabalin Patent Litigations raise basic Licensing Policy Questions? https://bit.ly/2zHTJky [Professor Elizabeth Goodman (Ref 44) found Ketorolac as good as Morphine with no respiratory depression in vaso-occlusive crisis but Lesner and Sally Davies said “Ketorolac has no product license in the UK for this indication” (Ref 45). How extraordinary that a drug that did not kill patients had no product license in the UK, BUT Morphine and Diamorphine that killed sickle cell disease patients as NCEPOD later confirmed [40 41] was, and still is licensed “for this indication”. Indeed, despite NCEPOD damning patients-dying-from-Opiate-Overdose Report NICE issued Guidelines advocating Diamorphine intravenously in sickle cell crisis [38]
47. Konotey-Ahulu FID. Current “hit and miss” care provision for sickle cell disease patients in the UK http://www.bmj.com/cgi/eletters/337/jul11_2/a/771#199135 BMJ
Rapid Response 16 July 2008. (Reference 31 describes how 2 Consultants in the same UK Teaching differ on prescription of opiates to sickle cell disease patients).
48.. Konotey-Ahulu FID. Clinicians facing conflicting recommendations. Use commonsense? http://ww.bmj.com/cgi/eletters/337/nov28_2/a2530#205377 December 2008.
49. Konotey-Ahulu FID. Valsalva vitreous haemorrhage and retinopathy in sickle cell haemoglobin C disease. Lancet 14 June 1997 Volume 349 No 9067, pp 1774.
50. Konotey-Ahulu FID. Gnathopathy – Grades 1, 2, 3. In chapter 14 of Ref 7 & 8 – The Sickle Cell Disease Patient – “Gnathopathy – a word coined by the author – (gnathos = jaw in Greek) to describe a peculiar overgrowth of the maxilla” commonest in ‘SS’ phenotype. Grade 1 is slight; Grade 2 is obvious. Grade three is grotesque – alsp seen in beta-Thalassaemua major. Which grade could Shaniqua have?
51. Konotey-Ahulu FID. Mental neuropathy, a complication of sickle ce3ll crisis. Lancet 1972; 2: 388. Been termed KANUMBLLL SIGN (Konotey-Ahulu Numb Lower Lip Lancet Sign – mentioned in next Lancet reference [47 below]
52. Konotey-Ahulu FID. Sickle cell disease and the patient. Lancet 2005; 365(9457): 382-383.
53. Konotey-Ahulu FID. Inferior Dental Nerve Symptomatology in Dental Practice Needs Exclusion of Sickle Cell Disease. Journal of Dental Problems and Solutions. Peertechz Publications 4 August 2022 https://www.peertechzpublications.com
54. Konotey-Ahulu FID. Epistasis from sickle cell disease must not be forgotten. BMJ Rapid response https://www.bmj.com/content/344/bmj.e1097/rr/576087 28 Mar 2012
55. Konotey-Ahulu FID. Torrential epistaxis associated with symmetrical facial skin ulceration in sickle cell anaemia. BMJ 1965; 2:859-860 doi:10.1136/bmj2.5466.859 http://www.bmj.com/cgi/reprint/2/5466/859.pdf
56. Konotey-Ahulu FID, Kuma Eunice. Skeletal crumbling in sickle cell anaemia complicated by Salmonella typhi infection. Brit J Clin Practice 1965; 19: 575-578. http://www.pubmedcentral.nih.gov/picender.fcgi?artid=1846577&blobtype=pdf
57. Konotey-Ahulu FID. Acute osteomyelitis in African children unmasks un-masks sickle cell disease with salmonellosis BMJ Rapid Response February 1 2014 http://www.bmj.com/content/348/bmj.g66?tab=response
58. Konotey-Ahulu FID. Gall stones in sickle cell disease. Page 175 in Refs 10 & 11
59. Archampong EQ. Biliary tract disease and sickle cell disease in Accra. In, Proceedings Gastroenterol Mex 1975; 40: 220.
60. Archampong EQ, Konotey-Ahulu FID. Biliary tract disease and sickle cell anaemia in Korle Bu Teaching Hospital in Accra. Ghana Medical Journal 1975; 13: 175-180.
61. Wosornu Lade, Konotey-Ahulu FID. Gastric secretion in sickle cell anaemia. Gut 1971: 12: 187-199. (Frequent abdominal pain is not always related to sickle cells).
62 Konotey-Ahulu FID. Leg ulcers in sickle cell anaemia Chapter 16 Sickle Cell Dermatopathy in Ghana, pages 196-198 in Refs 10 & 11 The Sickle Cell Disease Patient.
63. Acquaye CTA, Gbedemah KA, Konotey-Ahulu FID. Glucose-6-phosphate Dehydrogenase Deficiency Incidence in Sickle Cell Disease patients in Accra. Ghana Med J 1977; 16: 4-9 (Proper management must include establishing G6PD status. Treating urinary tract infection or pneumonia with a drug that exacerbates haemolysis and hepatopathy in the G6PD Deficient is bad medical practice, not only for Blacks but also for Greeks who have both sickle cell disease and G6PD Deficiency. [Reference 37]
64. Konotey-Ahulu FID. G6PD Deficiency in Ghanaians. How to recognise it. Click ‘BLOG’ on www.sicklecell.md and click on January 2008 for 20 answers.
65. Olujohungbe A, Cinkotal I, Yardumian A. Hydroxyurea therapy for sickle cell disease in Britain. BMJ Editorial 1998; 316: 1689. “Many patients are unwilling to take the drug and they vote with their feet.” (Dr Olujohungbe himself was “SS”)
66. Olujoungbe Ade. Bi-directional trust is needed in pain management in sickle cell disease. BMJ Rapid Response 2 July 1999 to Maxwell K, Streetly A, Bevan D BMJ 161.999; 318: 1585-1590.
67. Wise J. Crizanlimubab. Sickle cell disease: first new treatment in two decades becomes available in England. BMJ 4 Oct 2021;375: n2429 (Same therapeutic claim was made for Hydroxurea, but let those who have survived 15mg/kilogram bodyweight, ie 750 mg daily for a 50 kg person for 10 years write to BMJ. It is to be noted that the lead author of the BMJ Editorial Dr Ade Olujohungbe was a UK-trained Haematolgist who temporarily tried Hydroxyurea for his Sickle Cell Anaemia. (Reference 60 above). He honoured my Sickle Cell Disease Patient Achievers Conferences to prove that he had brilliant non-sickling genes that made him a post-graduate Specialist. Dr Samuel Charache MD, The Johns Hopkins University Specialist who introduced Hydroxyurea to the world was also at the International Conferences and expressed amazement at Ghanaian patients who had neither been transfused nor given Morphine or Diamorphine. What need have they for “Experimental life-changing drugs”?
68. Crizanlizumab UK National Haemoglobinopathy Panel – NHP Guidelines https://www.nationalhaemoglobinopathy-nhs.net Following NICE recommendation of Crizanlizumab as a treatment option for preventing recurrent crises (vaso-occlusive)
69. NHS UK News 5 Oct 2021 announces deal for lifechanging sickle cell treatment. “Crizanlizumab, the new drug will be delivered by a transfusion drip ‘’will help as many as 5000 people over the next three years to have a much better quality of life.”
70. NHS treats first sickle cell disease patients with life-changing drug. 24 Feb 2022 https://www.england.nhs.uk > nhs-tr (Total misinformation to call this “life-changing”).
71. West London HCC Adakveo (crizanlizumab) 10 mg/ml concentrate for solution for infusion. This is licensed for prevention of recurrent vaso-occlusive crises (VOC’s) in sickle cell disease patients aged 16 or more years. It can be given as an add-on therapy to hydroxyurea/Hydroxycarbamide (HU/HC) or as monotherapy in patients for whom HU/HC is inappropriate or inadequate. https://www.medicinesresources.nhs.uk https://www.westlondonhcc.nhs.uk (Licensed, but Ketorolac fraction the cost is not).
72 NHS. https://www.kch.nhs.uk > news 23 March 2022 [Photo of Black lady] King’s College Hospital: King’s patient is first to receive new sickle drug Crizanlizumab after it was approved for use across the NHS in November 2021 (How much does King’s College Hospital pay for opiates per year? And how much for this experimental drug?)
73. BBC https://www.bbc.com > news > health 24 Feb 2022 New sickle cell treatment given to first patients in England. Crizanlizumab, a monoclonal antibody, binds to a protein on blood cells, preventing them from clumping. Sickle cells mostly affects black people. (Discussing this with her doctor would Shaniqua agree to these injections?)
74. Konotey-Ahulu FID. Malaria and sickle cell: “Protection?” Or “No Protection?” – Confusion reigns. BMJ Rapid Response October 13, 2008 http://www.bmj.com/cgi/eletters/337/oct01_3/a1875#203067 [Felix Konotey-Ahulu’s brother Tei developed priapism (Ref 70) whenever malaria precipitated crisis]
75. Konotey-Ahulu FID. Sickle cell priapism. Chapter 19 (pp 226-235 / Refs 10 & 11)
76. Konotey-Ahulu FID. Comments on “Stem cells cure sickle cell anaemia in mice” http://www.sicklecell.md/blog/?=200712 Dec. 8, 2007. (Public Health Procedure?)
77. LentiGlobin – Experimental Gene Therapy Reverses Sickle Cell Disease for Years. Columbia University https://www.cuimc.columbia.edu > 13 Dec 2021 The new gene therapy called LentGlobin, blood-forming stem cells. Preventing them from clumping. Sickle cell mostly affects black people. (Would it be used on Greek patients too?) COVID-19 VACCINATION EFFECTS CAN AGGRAVATE SICKLE CELL DISEASE
78. Underdown M J, Nuss Rachelle. Thrombocytopenia in a teen with sickle cell disease following COVID-19 vaccination. Pediatric Blood Cancer 2021 Dec, 68;(12): 29271. Published on line 2021 July 31. doi: 10.1002/pbc.29271 PMCID: PMC8441926 PMID: 34331506 (Is it wise to prescribe COVID-19 vaccines for these patients?)
79. The BMJ https://casereports.bmj.com/content/15/5/e…Acute interstitial nephritis after COVID-19 vaccination WebA woman in her 70s presented to the hospital being generally unwell 8 days following the first dose of the AstraZeneca COVID-19 vaccination. She was in stage III acute kidney injury (AKI) with hyperkalaemia and metabolic …
80. NHS-https://www.nhs.uk/conditions/covid-19/covid-19-vaccination/ COVID-19 vaccines side effects and safety – NHS WebLike all medicines, the COVID-19 vaccines can cause side effects, but not everyone gets them. Most side effects are mild and should not last longer than a week, such as: You or …
81. PubMed https://pubmed.ncbi.nlm.nih.gov/35214760 New-Onset Kidney Diseases after COVID-19 Vaccination: A Case … Web16 Feb 2022 · In this study, we report the clinical courses and histopathologic findings of new-onset kidney diseases after COVID-19 vaccination as confirmed via kidney biopsy. Five patients aged 42 to 77 years were included in this study, and baseline kidney function was …
82.Underdown M J, Nuss Rachelle. Thrombocytopenia in a teen with sickle cell disease following COVID-19 vaccination. Pediatric Blood Cancer 2021 Dec, 68;(12): 29271. Published on line 2021 July 31. doi: 10.1002/pbc.29271 PMCID: PMC8441926 PMID: 34331506 (Is it wise to prescribe COVID-19 vaccines for these patients?) Keywords: COVID-19; IgA nephropathy; kidney biopsy; kidney disease; minimal change disease; thrombotic microangiopathy; tubulointerstitial nephritis; vaccination.
83. A case of fatal multi-organ inflammation following COVID-19 vaccination.Nushida H, Ito A, Kurata H, Umemoto H, Tokunaga I, Iseki H, Nishimura A.Leg Med (Tokyo). 2023 Mar 20;63:102244. doi: 10.1016/j.legalmed.2023.102244. Online ahead of print.PMID: 36990036 Free PMC article. A 14-year-old Japanese girl died unexpectedly 2 days after receiving the third dose of the BNT1262b2 mRNA COVID-19 vaccine. …In the present case, arrhythmia of atrial origin was assumed as the cause of cardiac failure and death. In sudden post …
84. Liver injury following SARS-CoV-2 vaccination: A multicenter case … Web31 Jul 2021 · Six patients had a history of chronic liver disease, including 4 (#6, 10, 11, 13) with autoimmune hepatitis (AIH) in treated remission (i.e., no medication changes or abnormal labs for a minimum of 6 months). Three patients had cirrhosis: 2 patients with …Author: Hersh Shroff, Sanjaya K. Satapathy, James M. Crawford, Nancy J. Todd, Lisa B. VanWagner
85. LIVER INJURY FOLLOWING COVID-19 mRNA VACCINE … WebBackground: The COVID-19 mRNA vaccines have been associated with infrequent reports of liver injury. The aim of this study is to describe the
presenting features, liver hist See more videos of Liver Failure After COVID-19 VACCINATIONLiver injury after SARS‐CoV‐2 vaccination: Features of … WebOne patient developed mild liver injury after a first dose of Pfizer‐BioNTech vaccine but presented with severe liver injury following a second dose of the same vaccine.
86. Coombes Rebecca. GMC challenged over anti-vax doctors. BMJ 2023;381: p1220 June 3, 2023 page 339.
NOTA BENE: Page 258 of my THE SICKLE CELL DISEASE PATIENT says “Whereas only 261 (44.2%) of 591 sickle cell anaemia (‘SS’) patients had no liver enlargement, a total of 77.8% of about the same number of sickle cell haemoglobin C disease (‘SC’) patients had no liver enlargement. [Refs 10 & 11]. If my assumption is correct that Mary Shaniqua is ‘SS’-phenotype, then she is likely to have some degree of hepatomegaly. Does she in fact? And was she ever advised to take a COVID-19 vaccine which we now know can badly affect the liver? If I advised (as I do now advise) that those with hereditary Erythrocytopathy (Sickle Cell Disease or/and G6PD Deficiency) should not be given COVID-19 Vaccines would I be in danger of being lumped into the so-called anti-vax doctors that Rebecca Coombes BMJ 3 June 2023, page 337 reports are being accused by some anonymous doctors of spreading Misinformation that needed probing by the GMC when they cautioned their patients against COVID-19 Vaccination? [86]