http://www.bmj.com/cgi/eletters/339/sep01_1/b3536#219836
Susan Mayor, 5 September, has done well to draw attention to 2 reports that reveal “the numbers of people dying because of poisoning from legal and illegal drugs are still increasing” [1] The first report said “Almost a third of the deaths where specific drugs were mentioned on the death certificate were related to heroin or morphine” [1, 2] The second report from St George’s University of London showed a 2.7% rise in the number of drug related deaths confirmed by inquest. Here too “Heroin and morphine accounted for most of these deaths” [3]. And these were the very drugs that the NCEPOD Report [4] found had produced deaths in sickle cell disease patients from overdose, and about which I continued to protest [5- 8].
HOW LONG WILL THIS CONTINUE FOR?
How long this situation is destined to continue is not clear. Writing to the Prime Minister and Health Ministers as I did, produced a response from
IS MY PROTEST JUSTIFIED OR NOT?
But why do I continue protesting like this? ANSWER: First of all, I did not train in the bush somewhere in
MY ADVICE TO NATIONAL INSTITUTE OF HEALTH AND CLINICAL EXCELLENCE
In the light of the above I make no apologies to take it upon myself to advise NICE to stop standing on the sidelines, and add to their many pronouncements one that forbids the “legal” use of Heroin (Diamorphine) for sickle cell disease patients. This, at least, was one thing NICE could learn from the
GENETIC COUNSELLING AND VOLUNTARY FAMILY SIZE LIMITATION
The real answer for now, and the future, as I have been saying for decades is Genetic Counselling and Family Planning [18, 19] warning my fellow Africans that if they did not check themselves for a beta-globin gene variant (an ACHE gene) they might suddenly find themselves with a child born with an ACHEACHE phenotype (ACHE from father and ACHE from mother), like Sickle Cell Disease, and “the genetic burden on the National Health Service will go up and up” [20]. If born in the
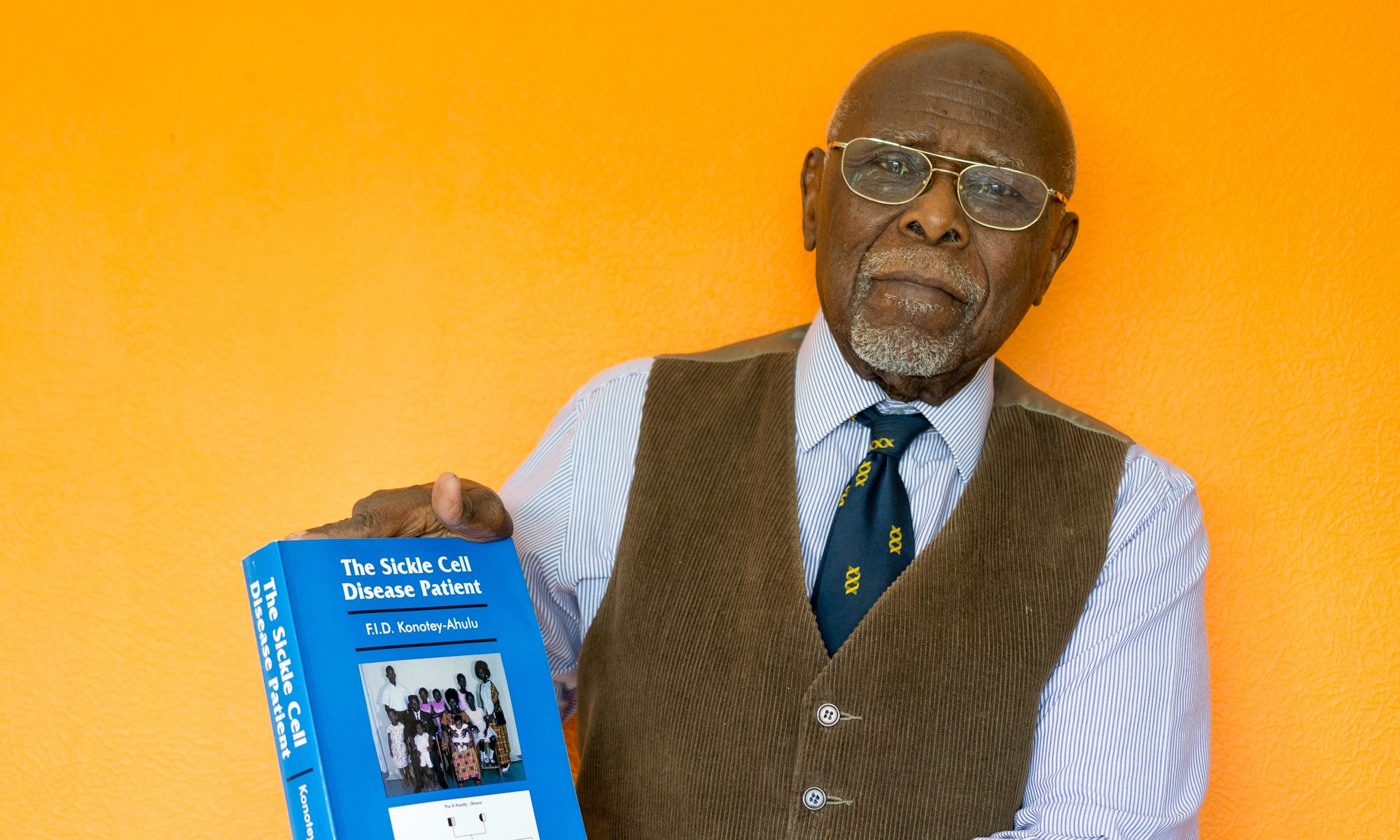
Felix I D Konotey-Ahulu MD(Lond) FRCP DTMH Dr Kwegyir Aggrey Distinguished Professor of Human Genetics, University of Cape Coast, Ghana and Consultant Physician Genetic Counsellor in Sickle & Other Haemoglobinopathies, 10 Harley Street London W1G 9PF.
felix@konotey-ahulu.com
1 Mayor Susan.
2 Deaths related to drug poisoning www.statistics.gov.uk/pdfdir/dgdths0809.pdf August 2009.
3 The
4 NCEPOD (National Confidential Enquiry into Patient Outcome and Death). SICKLE: A Sickle Crisis? (2008) [Sebastian Lucas (Clinical Co- ordinator), David Mason (Clinical Co-ordinator), M. Mason (Chief Executive), D Weyman (Research), Tom Treasurer (Chairman)] info@ncepod.org
5 Konotey-Ahulu FID. Poor care for sickle cell disease patients: This wake up call is overdue BMJ Rapid Response May 28 2008 BMJ 2008; 336: 1152 http://www.bmj.com/cgi/eletters/336/7654/1152a#196224 to Susan Mayor “Enquiry shows poor care for patients with sickle cell disease” on National Confidential Enquiry into Patient Outcome and Death (NCEPOD) REPORT “SICKLE: A Sickle Crisis? (2008) info@ncepod.org
6 Konotey-Ahulu FID. Current “hit and miss” care provision for sickle cell disease patients in the
7 Konotey-Ahulu FID. Management of sickle cell disease versus management of the sickle cell disease patient. http://www.bmj.com/cgi/elettrs/337/sep08_1/a1397#202088 BMJ Rapid Response 17 September 2008
8 Konotey-Ahulu FID. Inquest into diamorphine deaths: Does NCEPOD sickle patients report warrant a similar inquest? BMJ Rapid Response March 7 2009 http://www.bmj.com/cgi/eletters/338/mar03_3/b903#210208
9 Ballas SK. Sickle Cell Pain. IASP Press.
10 . Konotey-Ahulu, FID. Morphine for painful crises in sickle cell disease. BMJ 1991, 302(6792): 1604. (June 29 1991) (Comment on Professor Chamberlain's recommendation of morphine in pregnancy in sickle cell disease – BMJ 1991; 302: 1327-30.) doi:10.1136/bmj.302.6792.1604-c http://www.bmj.com/cgi/reprint/302/6792/1604-c.pdf PMID: 1855060 PubMed- indexed for MEDLINE
11 Konotey-Ahulu FID. Opiates for sickle-cell crisis? Lancet 1998; 351(9113): 1438. May 9. PMID: 9593444 PubMed-indexed for MEDLINE
12 Konotey-Ahulu FID. Opiates for sickle-cell crisis. Lancet 1998; 352(9128): 651-652. Aug 22. PMID:9746049 PubMed-indexed to MEDLINE
13 Konotey-Ahulu FID. Opiates for pain in dying patients and in those with sickle cell disease. 11 October 2007 BMJ Rapid Response http://www.bmj.com/cgi/eletters/335/7622/685#177986
14 Konotey-Ahulu FID. Sickle Cell Disease in successive Ghanaian generations for three centuries (Manya Krobo Tribe) In The Human Genome Diversity Project: Cogitations of An African Native. Politics and the Life Sciences (PLS) 1999, Vol 18: No 2, pp 317-322. http://www.konotey- ahulu.com/images.generation.jpg
15 Konotey-Ahulu FID. The Sickle-cell Diseases: Clinical manifestations including the Sickle Crisis. Arch Inten Med 1974; 133(4): 611-619. http://archinte.ama.assn.org/cgi/reprint/133/4/611-pdf or http://archinte.ama.assn.org/cgi/content/abstract/133/4/611 [PMID: 4818434 PubMed – indexed for MEDLINE]
16 Konotey-Ahulu FID. The sickle cell disease patient: natural history from a clinico-epidemiological study of the first 1550 patients of Korle Bu Hospital Sickle Cell Clinic. Watford Tetteh-A’Domeno Company 1996 & The Macmillan Press Ltd,
17 Konotey-Ahulu FID. Publications annually from 1965 to 2009 http://www.konotey-ahulu.com/publications_annual.htm
18 Konotey-Ahulu FID. Sickle Cell Disease: The Case for Family Planning.
19 Ringelhann B, Konotey-Ahulu FID. Hemoglobinopathies and thalassemias in Mediterranean areas and in
20 Konotey-Ahulu FID. Need for ethnic experts to tackle genetic public health. http://www.thelancet.com/journals/lancet/article/PIIS0140- 6736(07)61771-1/fultext Lancet 2007; 370: 1836 [doi:10.1016/50140- 6736(07)61771-1]
Competing interests: None declared.
Sickle Cell Disease Patients dying from Opiates: Why no co-operation among doctors? Mawunu Chapman Nyaho
http://www.bmj.com/cgi/eletters/339/sep01_1/b3536#220670 British Medical Journal 21 September 2009