Re: Should we abandon routine blood tests? No, not when hereditary erythrocytopathy poses a real problem in a so-called multi-racial population!
Should we abandon routine blood tests? No, not when hereditary erythrocytopathy poses a real problem in a so-called multi-racial population!
WEST AFRICANS NEED ERYTHROPATHIC TESTS BUT ONCE
The name “K Siau” [1] sounds Ghanaian from Kwahu Tribe, while the initial K could stand for any of the 7 Ghanaian Male Day-Names: Kwesi – Sunday to > Kwame – Saturday. [Our Kofi Annan was Friday-born]. If Siau is Ghanaian, then he may well be one of the “1 in 3 West Africans” who have inherited the abnormal haemoglobin gene ‘S’ or ‘C’, from one parent, not to mention the 1 in 4 males with Glucose 6 Phosphate Dehydrogenase (G6PD) Deficiency [2 3]. Millions of healthy West Africans in the UK have one gene for hereditary erythrocytopathy (abnormal haemoglobin S or C, plus or minus G6PD Deficiency) [4 5]. Routine blood tests performed just once can discern these [5]. UK is no longer entirely Caucasian therefore doctors need to unmask erythrocytopathy.
PROFESSOR MALCOLM MILNE AND THE CAUCASIAN’S SHOULDER
Orthopaedic Trainee Dr Alastair Faulkner [6] may have read my account [7] of a postgraduate ward round many years ago. After being asked to examine a white patient I gave my Clinical Impression: “This jaundiced Greek patient with pale nails, scars on one shoulder and right hypochondrium, and with limited straight leg elevation of right leg has avascular necrosis of the shoulder, avascular necrosis of one femoral head, and has had gall stones removed because of chronic haemolysis from Sickle Cell beta-Thalassaemia” [7] Duly impressed, Professor Milne produced laboratory results confirming my diagnosis proving that NOT ONLY BLACK PEOPLE SUFFER FROM SICKLE CELL DISEASE. In Greece, around Lake Kopais, the 30% incidence of sickle cell trait was higher than anywhere in Ghana [8-10]. Any new patient I ever had – Black, White, Hebrew, Asian or Indian must routinely have Haemoglobin Electrophoresis and G6PD test done and be given a Certificate of the findings.
PROBLEM WITH NHS TESTS
Dr Sam Lewis [11] mentions the “nit-picking rejection of lab requests” in the NHS. When Clinicians request certain tests, NHS Pathologists often decide which to accept and reject. While Locum Consultant Physician in a London Hospital I requested Haemoglobin Electrophoresis on a woman, only for the Pathologist to send a report: “Sickling Test Negative”. I protested I never asked for a Sickling Test; could I have Haemoglobin Electrophoresis, please? The Haematologist asked why if sickling test was Negative I wanted Haemoglobin Electrophoresis? I then told him I had in Ghana the largest collection of Homozygous Haemoglobin C Disease patients (CC) in the world (all sickling negative) and that it was a common cause of miscarriage in pregnant women [12] The Pathologist still refused to do the test so I sent the lady to a Private Lab where Haemoglobin CC Phenotype was confirmed. As husband was Sickle Cell Trait (AS) I counselled them, advising that they should expect to have Sickle Cell Disease (SC) and Haemoglobin C Trait (AC) offspring. [13]
DO ROUTINE TEST FOR GLUCOSE 6 PHOSPHATE DEHYDROGENASE DEFICIENCY
Do not wait till patients complain of “passing urine like coca cola”. Always testing new patients for Abnormal Haemoglobins and G6PD Deficiency was how we discovered that G6PD Deficiency was not just a haemolysis problem, but could aggravate the course of typhoid fever, renal failure, muscle pain, duration of coma from any cause, and the prognosis of sickle cell disease. [2 3 14 -20]. That was how we discovered the first ever African with zero G6PD enzyme in his red cells – a phenomenon thought only to exist in Mediterranean Caucasians. [21 22]. Ringelhann [23], Beutler [24], James Bowman and Robert Murray [25] confirmed high levels of G6PD Deficiency in Blacks on both sides of The Atlantic. Luzzatto, examining 100 “SS” males found 16% to be G6PD Deficient [26]. As salmonellosis is common in sickle cell disease [27 28], and Chloramphenicol is contraindicated in G6PD Deficiency, this test requires doing for all sickle cell disease patients [19].
QUANTIFICATION TESTS BETTER THAN QUALITATIVE BUT NOT CHEAP
Relying only on G6PD Colour Tests would have missed our zero-enzyme patients. Quantification is vital for both Abnormal Haemoglobin and G6PD enzyme. That was how we knew that Sickle Cell Traits have 3 modes of Haemoglobin S (20-25%, 30-35%, 36-39.5%) [29] which fact enables us to distinguish the true Sickle Cell Trait (“AS” with S less than 40%) from Sickle Cell beta-plus Thalassaemia Disease (2 abnormal genes) with Sickle gene product way above 50% [28 29 30].
WHO and International Atomic Energy Agency grants funded our tests. [5 28].
SHOULD ANYONE BE REFUSED THESE ONCE ONLY ROUTINE TESTS?
I have described a white Englishman (Hb D Trait) married to a Ghanaian lady (Hb S Trait) and their 2 sickle cell disease daughters (Ref 28, Illustrative Case History 133). If NHS budget is unable to sustain such a routine test burden shall we not ask enquirers to go Private for their health’s sake? Dr K Siau believes while we needed to “avoid unnecessary repetition of blood tests” [1] some routine tests “should be considered part of holistic Medicine …” [1]. Three out of every 100 West Africans in the UK have inherited TWO ABNORMAL HAEMOGLOBIN genes causing hereditary disease capable of showing up in any Clinical Discipline [See the 133 Illustrated Case Histories in Reference 28] not to mention the non-haematological complications of G6PD Deficiency [2 3 20 28 29]. I once expressed disappointment when a seven-part series on genetic epidemiology by “three white professors began in The Lancet on September 10, 2005” [30] only for the series to end without once mentioning the genetic burden of west Africans in the UK. [29]. Will Dr K Siau now add our West African statistics to those of the “4000 Danish patients” he produced [1]? As I said in 1982, we needed to “unearth the hundreds of cases of SC sickle cell disease, some of whom are bread winners, before they are brought in dying or dead in their first crisis for 10 years” [31]
Conflict of Interest: My Parents Heterozygote for Abnormal Hbns (“AC” & “AS”) had 11 children: 3 Sickle Cell Disease “SC”, 2 Heterozygotes “AC”, 2 Heterozygotes “AS”, 4 Homozygotes “AA” [32].
felix@konotey-ahulu.com Twitter@profkonoteyahul
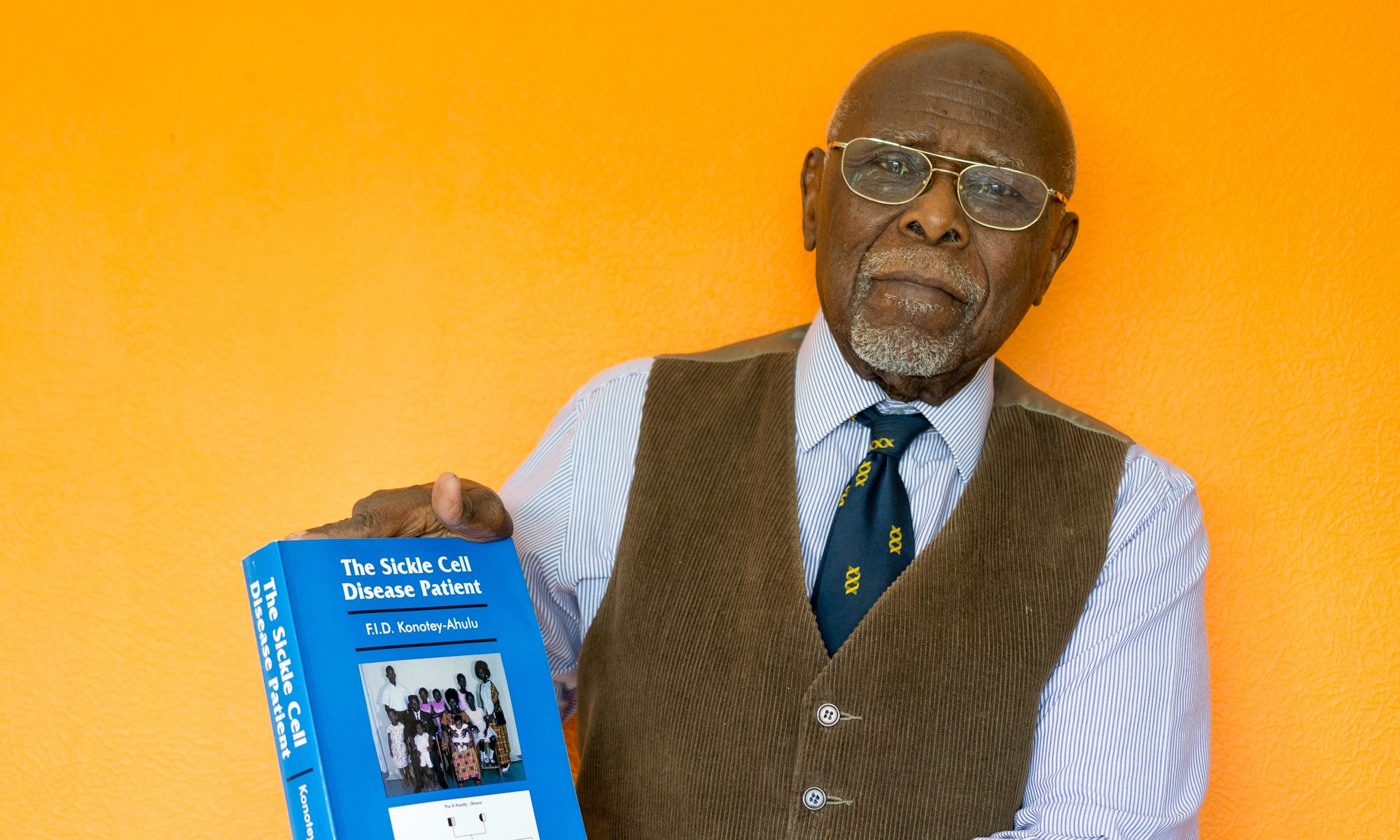
F I D Konotey-Ahulu MD(Lond) FRCP(Lond) FRCP(G) DTMH(L’pool) FGCP FWACP FTWAS
Kwegyir Aggrey Distinguished Professor of Human Genetics, University of Cape Coast, Ghana. Former Consultant Physician/Genetic Counsellor in Sickle & Other Haemoglobinopathies, Korle Bu Teaching Hospital, Accra, Ghana and at 9 Harley Street, London WIG 1AA. [ www.sicklecell.md ]
References
1 Siau K. Should we abandon routine blood tests? BMJ Rapid Response 8 May 2017. http://www.bmj.com/content/357/bmj.j2091/rr-6
2 Owusu SK. Glucose 6 Phosphate Dehydrogenase Deficiency in the causation of disease in Ghana. Ghana Med J 1974; 13: 168-170.
3 Konotey-Ahulu FID. Glucose 6 Phosphate Dehydrogenase Deficiency and Disease Causation in Ghana. (Editorial) Ghana Medical Journal 1974; 13: 155-158.
4 Ringelhann B, Dodu SRA, Konotey-Ahulu FID. Lehmann H. A survey for haemoglobin variants, thalassaemia, and Glucose 6 phosphate dehydrogenase deficiency in northern Ghana. Ghana Med J 1968; 17: 120-124.
5 Ringelhann B, Konotey-Ahulu FID. Hemoglobinopathies and thalassaemias in Mediterranean areas and in West Africa: Historical and other perspectives 1910 to 1997 – A Century Review. Atti dell’Accademia dell Science di Ferrara (Milan) 1998;74: 267-307
6. Faulkner Alastair, Reidy Mike, McGowan James. Should we abandon routine blood tests? BMJ 2017; 357: j2091 www.bmj.com/content/357/bmj.j2091?sso=
7 Konotey-Ahulu FID. Hip pain and radiographic signs of osteoarthritis: Sickle cell and other haemoglobinopathy differential diagnosis. BMJ Rapid Response 8 January 2016 http://www.bmj.com/content/351/bmj.h5983/rr-2
8 Choremis G, Sickle cell anaemia in Greece. Lancet 1951; 1: 1147.
9 Choremis G. Sickle cell trait and blood groups in Greece. Lancet 1953; 2: 901-911.
10 Delyannis GA, Tavlarakis N. Sickling phenomenon in Northern Greece. BMJ 1955; 2: 299-301.
11 Lewis Sam. Should we abandon routine blood tests? BMJ Rapid Response May 4 2017 www.bmj.com/content/bmj.j2091/rapidresponses
12 Konotey-Ahulu FID. Homozygous Haemoglobin C Disease. In FID Konotey-Ahulu. The spectrum of phenotypic expression of clinical haemoglobinopathy in West Africa. New Istanbul Contribution to Clinical Science 1978 Dec; 12(3-4): 246-257.
13 Konotey-Ahulu FID. SICKLE CELL DISEASE: The Case for Family Planning. Astab Books Ltd., Accra Ghana 1973.
14 Owusu SK. Clinical manifestations of glucose 6 phosphate dehydrogenase (G6PD) deficiency in Ghana. Ghana Medical J 1978; 17: 235-239.
15 Owusu SK, Foli AK, Konotey-Ahulu FID, Janosi M. Frequency of Glucose 6 Phosphate Deficiency in typhoid fever in Ghana. Lancet 1972; 1: 320.
16 Adu D, Anim-Addo Y, Foli AK, Yeboah ED, Quartey JKM. Acute renal failure and typhoid fever. Ghana Medical Journal 1975; 14: 172-174.
17 Owusu SK, Addy JH, Foli AK, Janosi Marianne, Konotey-Ahulu FID, Larbi EB. Acute reversible renal failure associated with glucose 6 phosphate dehydrogenase deficiency. Lancet 1972; 1: 1255-1257.
18 Konotey-Ahulu FID. Glucose 6 phosphate dehydrogenase deficiency and sickle cell anaemia. New Eng J Med 1972; 287: 887-888.
19 Acquaye CTA, Gbedemah KA, Konotey-Ahulu FID. Glucose 6 phosphate dehydrogenase deficiency incidence in sickle cell disease in Accra. Ghana Med J 1977; 16: 4-7.
20 Konotey-Ahulu FID. G6PD Deficiency in Ghanaians: How to recognize it. http://blog.konotey-ahulu.com/blog/_archives/2008/1/16/3458557.htmlJan. 16 2008.
21 Owusu SK. Absence of glucose 6 phosphate dehydrogenase (G6PD) in red cells of an African. BMJ 1972; 4: 25-26
22 Owusu SK, Opare-Mante A. Electrophoretic characterization of glucose 6 phosphate dehydrogenase (G6PD) enzyme in Ghana. Ghana Medical Journal 1972; 11: 304
23 Ringelhann Bela. A simple laboratory procedure for the recognition of the A (African Type) G6PD Deficiency in acute haemolytic crisis. Clin. Chim. Acta 1972; 36: 272-274.
24 Beutler E. Genetic Disorders of Red Cell Metabolism. Medical Clinics of North America 1969; 53: 813-826.
25 Bowman James E, Murray Robert F. Genetic Variation and Disorders in Peoples of African Origin. The Johns Hopkins University Press Ltd, London 1990, pp 171-190.
26 Luzzatto Lucius. G6PD Deficiency frequency and sickle cell association on the African continent. INSERM 1975; 44: 229.
27 Konotey-Ahulu FID, Kuma Eunice. Skeletal crumbling in sickle cell anaemia complicated by Salmonella Typhi infection. British J Clin Practice1965; 575-578.
28 Konotey-Ahulu FID. The Sickle Cell Disease Patient. Natural History from a clinico-epidemiological study of the first 1550 patients of Korle Bu Hospital Sickle Cell Clinic. T-A’D Company Watford 1996 [First Published 1991 & 1992 The Macmillan Press Ltd., London and Basingstoke] – 643 pages. [This book has 133 Illustrated Case Histories not found elsewhere]
29 Konotey-Ahulu FID. Alpha-Thalassaemia nomenclature and abnormal haemoglobins. Lancet 1984; 1: 1024-1025.
30 Weatherall DJ, Clegg JB. The Thalassaemia Syndromes 1981. Third Edition, Blackwell Scientific. Oxford.
31 Konotey-Ahulu FID. Survey of sickle cell disease in England and Wales. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1495623/pdf/bmjcred00588-00…
BMJ 1982; 284: 111 (January 9)
32 Konotey-Ahulu FID. Sickle Cell Disease in Successive Ghanaian Generations for Three Centuries (Manya Krobo Tribe) Chapter 2 Reference 28 pp 6-20, and FID Konotey-Ahulu in The Human Genome Diversity Project: Cogitations of An African Native. Politics and The Life Sciences (PLS) 1999; Vol 18: No 2, pp 317-322 [Invited Commentary on Professor David Resnik’s article: The Human Genome Diversity Project: Ethical Problems and Solutions]
Competing interests: My Parents Heterozygote for Abnormal Hbns (“AC” & “AS”) had 11 children: 3 Sickle Cell Disease “SC”, 2 Heterozygotes “AC”, 2 Heterozygotes “AS”, 4 Homozygotes “AA” [32].